By Dr. Brandon Colby MD, a medical expert specializing in personalized preventive medicine and clinical genomics.
Coronavirus treatment has evolved over the last year as scientists learn more about the pandemic that has taken over the world.
COVID-19 continues to spread as healthcare organizations such as the Centers for Disease Control and Prevention (CDC.gov) warn people to remain at least six feet apart and wear masks in public. SARS-COV-2 has led to hospitalizations for many people with severe COVID-19 outcomes, and unfortunately, many have not recovered.
COVID-19 Treatments Options

The good news is most people who contract novel coronavirus recover, even hospitalized patients with severe cases of the illness. One of the reasons is because of antiviral drugs.
Healthcare providers have several options when treating severe illnesses such as 2019-nCoV. The following are how medical professionals have been treating COVID-19 infection.
VEKLURY® Remdesivir - Antiviral Drug
The United States Food and Drug Administration (FDA) approved the antiviral drug remdesivir in October 2020 for coronavirus treatment. Clinical trials of the drug have shown that patients recover much faster with this treatment.
Bamlanivimab and Casirivimab/Imdevimab - Antibody Treatments
A month after the US Food and Drug Administration approved remdesivir in November, two monoclonal antibody treatments bamlanivimab and a combination of casirivimab and imdevimab were also approved with emergency use authorization in the US and EUA. These coronavirus treatments were approved for outpatient use. Clinical trials for these drugs suggest a reduction in hospitalization and emergency room risks. Although, these COVID-19 treatments need to be given intravenously (by IV) as soon as symptoms develop.
Dexamethasone - Corticosteroid (Anti-Inflammatory)
Another treatment for coronavirus clinicians recommend is a corticosteroid drug dexamethasone - an anti-inflammatory. The risk of death was lower for COVID-19 patients who were treated with this drug in a recent report published in a medical journal. Medical experts believe the drugs reduce the overreaction of the immune system, which is believed to damage the lungs and other organs - not necessarily the coronavirus. This implies the best time to start this coronavirus treatment is when the immune system starts to go into overdrive, which is the cause of the cytokine storm.
Chloroquine or Hydroxychloroquine/Azithromycin
When the COVID-19 pandemic first started, some doctors believe patients improved quicker with chloroquine or hydroxychloroquine (with azithromycin at times). These drugs have treated malaria and inflammatory diseases, such as lupus and rheumatoid arthritis in the past effectively.
Despite the positive effects of using chloroquine or hydroxychloroquine/azithromycin, many medical experts are not convinced they are the best coronavirus treatment. Azithromycin is an antibiotic that doesn't normally have an effect on viral infections, but since it does have an anti-inflammatory effect on the body, it could be treating symptoms of COVID-19.
Vitamin C
COVID-19 patients in intensive care have been treated with high doses of intravenous (IV) vitamin C. Unfortunately, while this has helped some people, it is still not considered the first course of action. A study currently being conducted in China is evaluating the treatment for severe COVID-19 and results are anticipated for Fall 2021.
Supplemental Oxygen - Mechanical Ventilation
The public health organization National Institutes of Health (NIH) released COVID-19 treatment guidelines to include supplemental oxygen by way of mechanical ventilation for coronavirus treatment. A decline in oxygen levels is a consequence of the COVID and many patients have recovered with the help from oxygenation.
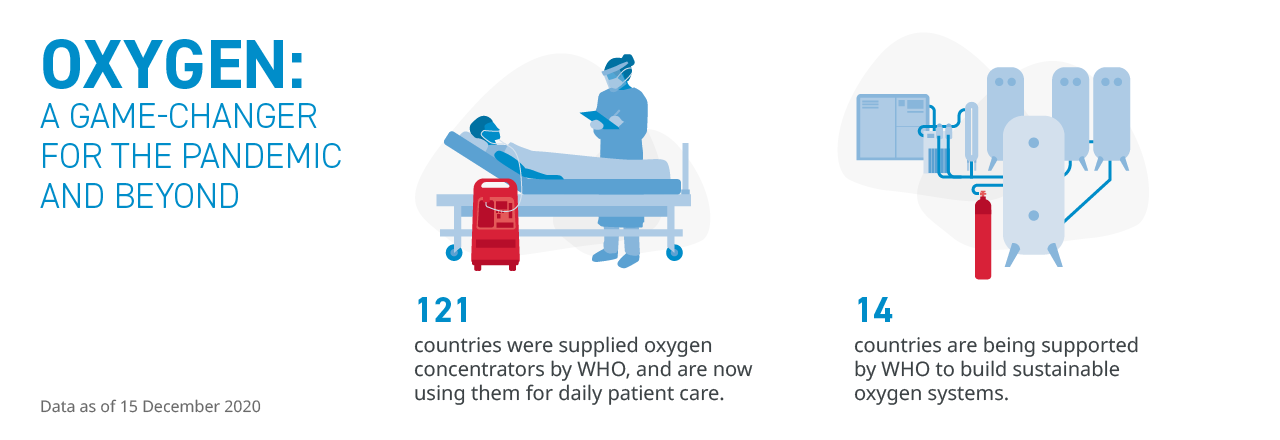
Photo Credit: World Health Organization
Convalescent Plasma
People who recover from infectious diseases such as ebola and COVID-19 have blood that contains antibodies that can fight the disease. The antibodies are part of blood plasma. Convalescent plasma is the name plasma from recovered coronavirus patients has been given. A blood transfusion transfers the plasma to someone who is fighting the illness to decrease the severity.
Over-the-Counter Coronavirus Treatment
Healthcare professionals recommend acetaminophen (Tylenol) for fever and body aches. Antihistamines like Claritin and Allegra can relieve nasal congestion and an apple cider vinegar rinse can calm a sore throat. To speed up recovery, the antioxidant glutathione seems to work well. It can be found in spinach, asparagus, and broccoli.
Symptoms of COVID-19

Early treatment of COVID-19 can reduce outcome severity. Be aware of the following symptoms:
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Muscle or body aches
- Headache
- New loss of taste or smell
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
- Diarrhea
Seek medical care as soon as the above symptoms present, especially if you're part of a high-risk population:
- Older than 65 years of age.
- Pre-existing medical conditions.
Higher-risk individuals may be more prone to COVID-19 vaccine to do an inhibited immune response and may suffer from life-threatening complications.
COVID-19 Treatment Side Effects
The coronavirus disease 2019 has led to new medical treatments and the resurface of older ones. Side effects from the treatments and medications for COVID-19 have been a concern for many people.
Medication side effects have a lot to do with people's genetic makeup, explained in this article.
Genetic testing can expose the risks of side effects as well as the best medications for different diseases and illnesses. This information can help you reduce side effects of medicine. Not only is it good for people to know the effects of treatments or medications, but it can be used by healthcare professionals to quickly decide on the right medication at the right dose.
Click here to learn more about how you can learn about the effects of medicine on the body.
Additional Information About Coronavirus and DNA
Coronavirus and DNA have been receiving a great deal of attention lately. You can learn more about it by reading about Blood Type and COVID: Infection Risk and Severity and Where Can I Get My Blood Type Checked for Free.
About The Author
Dr. Brandon Colby MD is a US physician specializing in the personalized prevention of disease through the use of genomic technologies. He's an expert in genetic testing, genetic analysis, and precision medicine. Dr. Colby is also the Founder of Sequencing.com and the author of Outsmart Your Genes.
Dr. Colby has performed extensive research pertaining to how coronavirus causes infection. Dr. Colby describes his COVID-19-related research in the article Your DNA and Coronavirus: How To Know If You're At Risk.
Dr. Colby holds an MD from the Mount Sinai School of Medicine, an MBA from Stanford University's Graduate School of Business, and a degree in Genetics with Honors from the University of Michigan. He is an Affiliate Specialist of the American College of Medical Genetics and Genomics (ACMG), an Associate of the American College of Preventive Medicine (ACPM), and a member of the National Society of Genetic Counselors (NSGC).